Community pharmacies successfully recruited adolescent girls and young women at risk for HIV and other sexually transmitted infections by tailoring their engagement strategies and being adaptable.
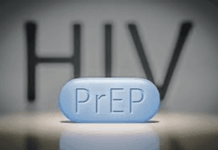
Adolescent girls and young women in sub-Saharan Africa have access to pre-exposure prophylaxis (PrEP) and HIV self-testing but are underutilizing them. They also have high incidence of HIV, other sexually transmitted infections, and unwanted pregnancies. Community pharmacies, where adolescent girls and young women readily access emergency contraception, are an underutilized resource to expand the delivery of HIV-prevention.
From May to December 2022, the investigators mapped community pharmacies within 45 km of one research clinic in peri-urban Kampala, Uganda, to assess the willingness, readiness, and feasibility of integrating PrEP delivery with emergency contraceptive services. They encouraged pharmacy providers to identify and refer the adolescent girls and young women who sought emergency contraception services to the research clinic for study screening. The researchers also documented challenges faced during the recruitment of potential study participants.
Ten of 15 community pharmacies participated in the study, referring 162 candidates for screening. Of these, the study excluded 32 participants due to age limits, lack of interest, not having time, or not using emergency contraception.
For the 130 enrolled participants, recruitment challenges included 1.) difficulty obtaining contact information from the girls and women who visited the pharmacy for emergency contraception without further interaction, 2.) provider reluctance to disclose individuals’ use of emergency contraception, 3.) the physical difficulty for research assistants to visit certain pharmacies that limited their outreach efforts, 4.) incorrect contact information for participants that hindered follow-up activities, 5.) cultural barriers that inhibited provider-client discussions about sexual behaviors, 6.) lack of interest or time, and 7.) being over 24 years of age.
To tackle these challenges, the authors implemented several strategies: improving communication and building rapport with pharmacy providers to improve comfort and accuracy in referrals; focusing weekend outreach efforts to better accommodate the adolescents and young women who were unavailable during the weekdays due to work or school; and developing targeted communication approaches to alleviate cultural discomfort and hesitancy when discussing sexual health.
The authors advise that future studies should adopt holistic, culturally sensitive, and collaborative approaches to increase HIV preventive uptake by adolescent girls and young women.
Reference
Nalumansi A, et al. IAS 2025. E-Poster EPO392